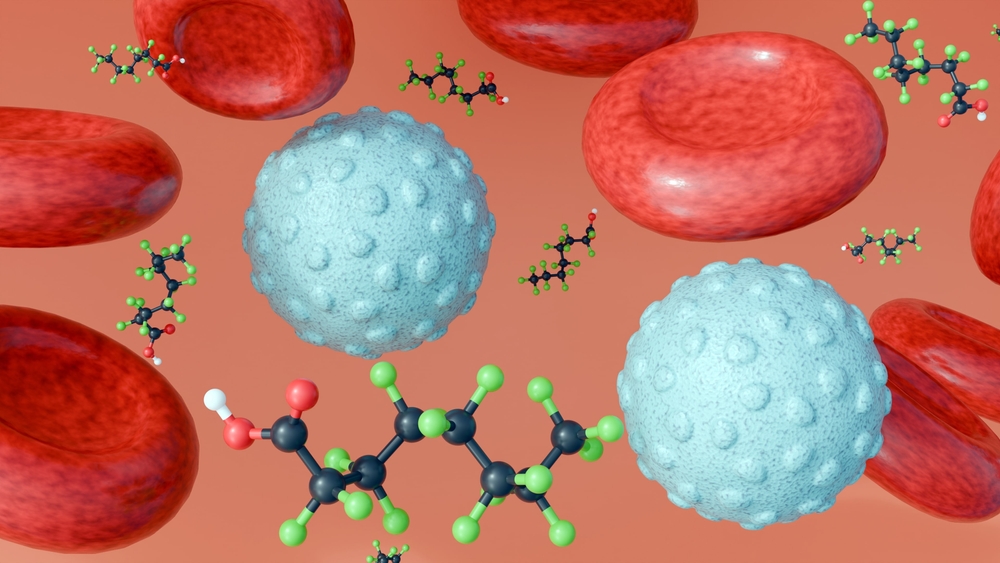
As part of a national environmental health assessment, the PFAS blood test program detected widespread exposure across US populations.
According to the Centers for Disease Control and Prevention (CDC), data from the National Health and Nutrition Survey (NHANES) show that most Americans can detect PFA exposure in their blood.
These findings stem from years of research and are published in the CDC National Report on Human Exposure to Environmental Chemicals.
“PFAs can stay in the body for years, and blood tests are often the only way people will notice that they have been exposed,” explained Sarah Miller, the legal assistant for the Legal Request Assistant, advocating for PFAS blood tests.
“PFAS blood tests provide a more clear picture of exposure levels for individuals and communities and can inform both medical surveillance and environmental policy.”
Causes of high levels of PFA exposure
The Environmental Protection Agency (EPA) identifies common sources of PFA exposure, including drinking water, food packaging, industrial emissions, and consumer products.
Individuals in close proximity to a military facility, airport, or facility using fluorescent chemicals may be at higher risk due to legacy contamination or occupational exposure.
Health outcomes depend on many factors, but several scientific studies have investigated the association between PFA exposure and specific health effects. These include potential links to altered liver function, disruption of thyroid hormone levels, and reduced vaccine response.
“For individuals with medical concerns associated with elevated PFAS levels, PFAS blood test data may support informed discussions with healthcare providers,” Miller said.
How PFAS blood tests can help you detect
PFAS blood tests usually involve testing specific compounds such as PFOA, PFOS, and Genx.
The accredited laboratory analyzes blood samples to quantify PFA concentrations in a billion (PPB) portion. These tests are often performed by government health agencies, occupational health researchers, or private clinics in areas where exposure is known.
The Toxic Substances and Disease Registry (ATSDR) notes that biomonitoring has not determined whether PFA exposure caused the disease. However, elevated levels may support further medical evaluation and risk communication.
Source link