Sona founder and CTO Dan Sarno has deployed a mobile breast density monitoring device aimed at enhancing breast cancer detection.
When it comes to breast cancer detection, breast density is extremely important when it comes to breast cancer detection, as breast cancer increases the risk of breast cancer and can miss cancer screening. Nevertheless, most women do not recognize breast density.
With a focus on breast density and aimed at revolutionizing breast cancer screening, National Physical Laboratory (NPL) Spinout Sona has developed the world’s first ultrasound-based breast density assessment and surveillance technology that does not require imaging or trained radiologists.
SONA’s technology allows healthcare providers to provide timely and personalized screening through simple, secure, low-cost access to breast density information currently restricted by the age and use of traditional mammograms.
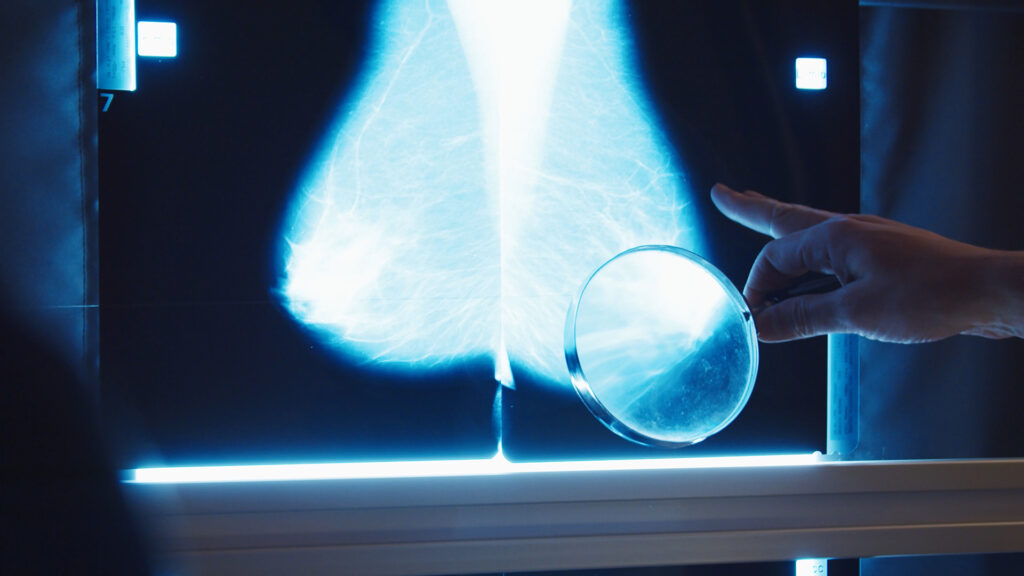
Unlike traditional methods that rely on x-rays, SONA’s patented solutions leverage new ultrasound sensor platform technology to provide a safer and more sensitive breast density rating. SONA’s simple, low-cost desktop devices are easily deployed to local GP clinics and primary care sites, providing fast and reliable breast density measurements.
For more information about Sona’s innovation, the Innovation Platform spoke to CTO Dan Sarno, founder.
Can you explain breast density and why it is so important to recognize breast density in relation to cancer detection?
Breast density refers to the proportion of fibre (dense) tissue compared to breast adipose tissue. Its most pressing impact lies in how clearly cancer is seen in mammograms. Both the dense tissue and the tumor appear white on the mammogram. This makes it difficult to spot cancers hidden in dense areas. This is known as “masking.”
This is a major screening issue. Research shows that up to half of cancer can be overlooked in women with dense breasts during daily mammograms. These are not unusual outliers either. Approximately 40-50% of women over the age of 40 are dense, with even higher prevalence among women in their 30s and 40s.
Beyond masking, breast density is also an independent risk factor. Women with extremely dense breasts can be up to six times more likely to develop breast cancer than women with less dense density. Nevertheless, breast density is not routinely measured or reported in the UK screening programme, so millions of women are unaware that they are facing both increased risk and the benefits of standard screening.
How can breast density information provide better screening services?
Once breast density is known, it is possible to personalize screening to individuals rather than relying on a single size approach. This is already part of Europe and is happening all over the United States. Women may be informed of breast density on a daily basis and may be provided with additional images such as ultrasound or MRI if at high risk.
Although the UK has not yet adopted this model, recent evidence suggests that it could have a significant impact. A British study found that providing alternative additional scans for mammograms for women with dense breasts could detect more cancers faster and save around 700 lives a year. Without knowing who has a dense organization, these women do not look effective in the system.
Bringing density into regular screenings will allow the NHS to make better informed decisions. This will help target enhanced screening when needed most and bridge the current gap in early detection.
What are the premises of SONA’s ultrasound technology?
These developments are that there is no practical, routine method for measuring breast density. Mammograms can provide estimates of density, but this has not been consistently measured and is rarely used to inform risk or follow-up care.
Without a reliable and accessible way to measure population density, opportunities for improved surveillance, early detection, and service planning are overlooked.
In response to this challenge, the future spin-out of the UK National Institute of Physics (NPL) (known as SONA) is developing a new approach. We are working on compact, ultrasound-based devices designed to safely, objectively, and across hospitals to assess breast tissue composition safely and objectively in the environment.
How is the technology developed?
Sona aims to provide a safe, consistent and accessible way to assess breast density, combining both reliable measurements and a comfortable experience. This is clearly different from the pain associated with mammograms.
The fundamentals of technology are rooted in measurement science. The device uses ultrasound to extract quantitative measurements of breast tissue composition related to breast density. SONA’s technology development is based on over a decade of research at NPL, including innovations in patent-protected sensors and new measurement methods.
The system has also been developed in consultation with women and clinicians to make it comfortable and easy to use. By combining measurement science with co-designed product development, SONA is committed to a tool that will quickly provide reliable measurements and allow women to feel more sympathy.
What stages are development and what is the purpose of using the technology (key users and when)?
The technology is currently in the preclinical stage, with working prototypes being improved prior to initial human testing. The core components have been demonstrated in the lab, and the team is working with NHS partners to prepare healthy volunteer research. These evaluate the performance and ease of use of the system prior to large-scale research.
The development is supported by the Government’s Technology Transfer Authority (GOTT) and the UK Innovation and Science Seed Fund (UKI2S) to support advances in technology beyond research and application use. This involves advancing both the device itself and the surrounding clinical and regulatory pathways.
In the long run, the system is designed for use in a community-based setting by trained medical staff, including nurses, screening practitioners and primary care teams. Its aim is to support faster, safer, and more comprehensive breast health assessments, especially for women who are not currently blessed with existing routes.
What advantages can Sona devices have over current screening methods?
Current breast screening is a one-size-fits-all approach that focuses primarily on mammography, with limitations, especially for women in densely populated tissues and women considered average risk. SONA’s technology could enable different approaches. A screening program suitable for high-risk women or women with dense breast tissue through accessible measurements outside the hospital environment, personalized risk-based risks with earlier ages to more dense breast tissue.
The system is small, low cost, and designed to be operator-independent, making it easy to identify women who may benefit from tailored screening and further surveillance, as it can be used early in community settings and life. This is particularly relevant to groups that are often underrepresented in current screening services, including young women and women from underserved communities.
By providing a consistent and accessible measurement of breast tissue characteristics, SONA’s technology supports more personalized screening pathways, contributes to previous identification of people at increased risk, and helps bridge detection gaps without replacing existing imaging methods.
This article will also be featured in the 23rd edition of Quarterly Publication.
Source link