If you feel like throwing up or have acid reflux, you may feel a burning sensation as the acid escapes into your esophagus. But if stomach acid is strong enough to irritate the lining of your throat, why doesn’t it pass through your stomach?
The human stomach has evolved to create and withstand extremely corrosive conditions. “Its role is to break down the physical food components into smaller pieces, and the idea is that by the time the preparation reaches the small intestine, it’s in small enough components that it can be absorbed,” Dr. Sally Bell, a gastroenterologist at Monash University in Australia, told Live Science.
you may like
Dr. Benjamin Levy III, a gastroenterologist at the University of Chicago Medicine, said this harsh environment also has a secondary protective role. “Gastric juices also help the body kill bacterial pathogens, keep us from getting sick, and strategically prevent bacterial overgrowth from occurring,” Dr. Levy told Live Science. This is especially important to destroy potential foodborne pathogens, he said.
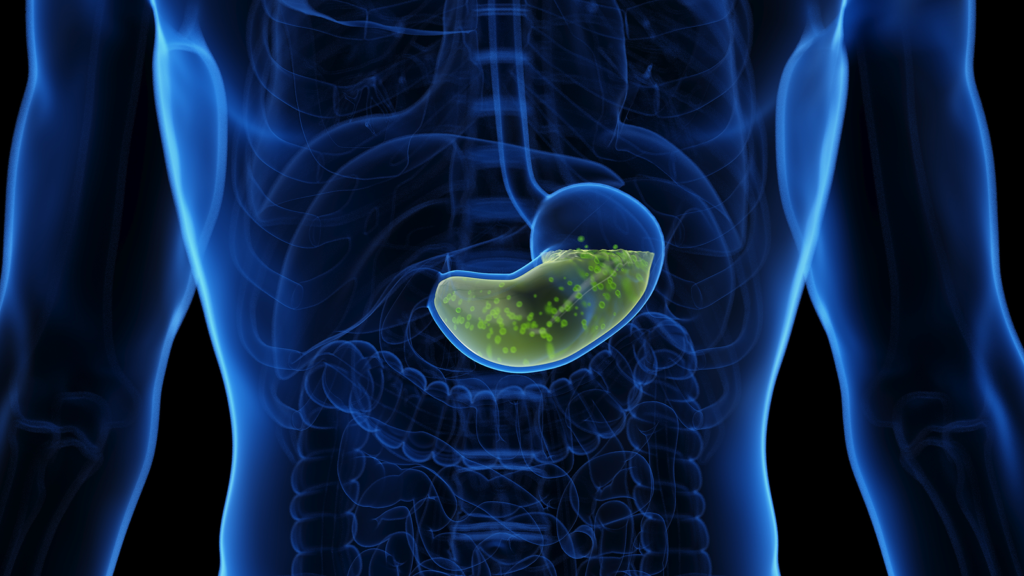
Without protection, this combination of strong acids and protein-digesting enzymes quickly begins to erode the stomach wall, first forming painful ulcers and eventually burning and puncturing. However, the cells lining the stomach (a layer known as the epithelium) have developed special secretions to protect the organ from attack.
“These cells are unique in that they produce a very thick sticky mucus layer that is alkaline and buffers acids,” Bell explained. “Because it is essentially a bicarbonate-rich proteinaceous substance, it protects the stomach lining from the stomach’s own acids and enzymes.”
In a healthy digestive system, this mucosal barrier lines the stomach wall and is continually renewed by epithelial cells to provide continued protection. However, problems can occur if the layers are damaged. Professor Levy said even small cuts can allow acid and pepsin to get under the mucus, causing chronic inflammation and ulcers.
One cause of such damage is the overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. “NSAIDs damage the stomach lining by inhibiting cyclooxygenase (COX-1), an enzyme involved in the production of hormone-like compounds called prostaglandins,” Dr. Levy said.
“This reduces prostaglandin production, which reduces both mucus and bicarbonate secretion,” Dr. Levy explained.
Bell pointed out that certain lifestyle choices, such as smoking and drinking alcohol, can also increase the risk of this type of digestive disease because they act as toxins directly on the lining of the body. Additionally, acidic or spicy foods can overwhelm the stomach’s natural protective functions, causing inflammation and reflux into the esophagus.
Despite extremely acidic conditions, bacterial infections can cause stomach problems. For example, “Helicobacter pylori has the ability to secrete proteases and lipases that break down gastric mucus and harm the phospholipid layer on the surface of the epithelium,” Professor Levy said. If H. pylori is detected, it can be treated with a combination of antibiotics.
The bottom line? Because stomach acid plays an essential role in digestion and defense against disease, this organ has developed an amazing ability to protect itself and regenerate its lining.
This article is for informational purposes only and does not provide medical advice.
Source link