An image-only artificial intelligence (AI) model for predicting five-year breast cancer risk provided stronger and more accurate risk stratification than breast density assessment, according to a new study.
Constance Lehman, lead author and professor of radiology at Harvard Medical School, said traditional methods of assessing a woman’s breast cancer risk, such as age, family history, genetics and breast density, are inadequate.
“More than 2 million women are diagnosed with breast cancer each year, and for most it’s a complete shock,” she says.
“Only 5 to 10 percent of breast cancer cases are thought to be hereditary, and breast density alone is a very weak predictor of risk.”
Use AI to monitor patterns in breast tissue that experts can’t see
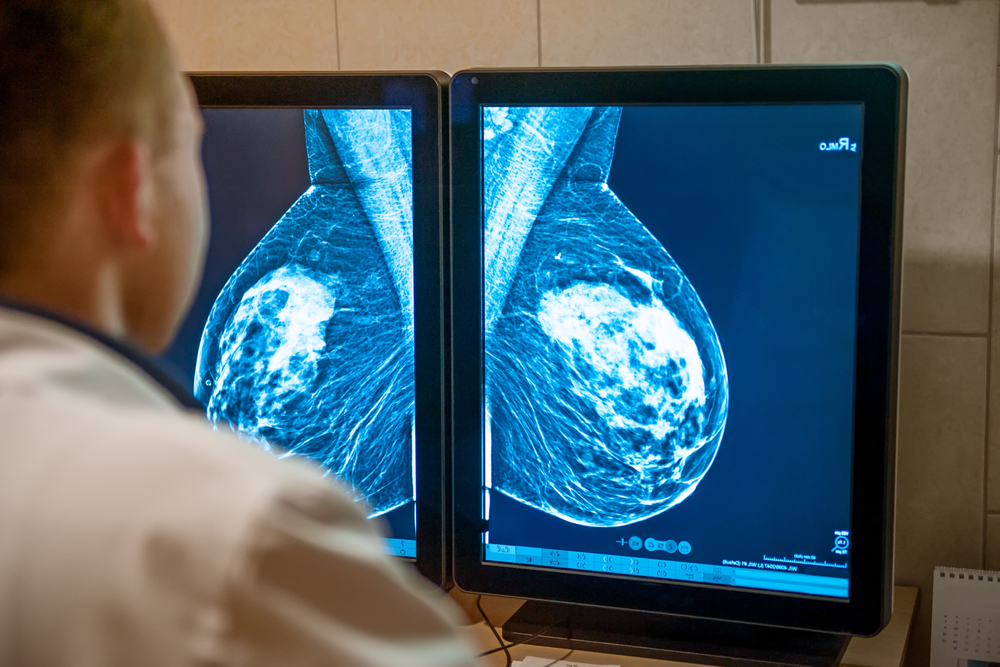
Clairity Breast is the first image-only AI breast cancer risk model cleared by the FDA and was trained on 421,499 mammograms from 27 sites in Europe, South America, and the United States.
By using mammograms from both women who developed cancer and women who did not develop cancer over the next five years, the AI model was able to learn patterns and differences in breast tissue that predict breast cancer risk.
The model was calibrated on an independent test set using a deep convolutional neural network to generate 5-year risk probabilities.
Dr. Lehmann explained: “This model can detect changes in breast tissue that are invisible to the human eye, a task that radiologists cannot perform.”
“This is a separate task from detection and diagnosis, and it leverages the power of AI and untapped information in images to open up a whole new field of medicine.”
Density monitoring alone is not enough to adequately predict breast cancer risk
The model was applied to a study group of 236,422 bilateral 2D screening mammograms from five centers in the United States and 8,810 from one center in Europe.
Radiologist-reported breast density (dense or not) and 5-year cancer outcomes were extracted from medical records and tumor registries, respectively.
AI-predicted risk was categorized as average (<1.7%), moderate (1.7–3.0%), and high (≥3.0%) according to National Comprehensive Cancer Network thresholds.
The researchers compared risk categories using a statistical model that took into account follow-up time and censoring.
When breast density was taken into account, women in the high-risk AI group had more than four times the cancer incidence than women in the average-risk group (5.9% vs. 1.3%). In contrast, breast density alone showed only moderate separation (3.2% for dense and 2.7% for non-dense).
“The results of this large-scale analysis show that the AI risk model provides a much more powerful and accurate risk stratification for five-year cancer prediction than breast density alone,” said lead author and presenter Christian Kuhl, Head of the Department of Diagnostic and Interventional Radiology at RWTH Aachen University Hospital.
“Our findings support the use of image-only AI as a complement to traditional markers to support a more personalized approach to breast cancer screening.”
Determine who needs screening at an earlier age
The American Cancer Society currently recommends that women at average risk for breast cancer have the option of starting annual mammography screenings at age 40.
However, women under 40 are the fastest growing group to be diagnosed with breast cancer and advanced disease.
“AI image-based risk scores can help identify high-risk women more accurately than traditional methods and determine who needs early screening,” Dr. Lehman commented.
“We are already screening women in their 30s who are clearly at high risk based on family history and genetics. In the future, a baseline mammogram at age 30 could allow women with high image-based risk scores to participate in earlier, more effective screening pathways.”
The future of breast cancer risk identification
Breast density laws in 32 states require health care providers to notify women undergoing mammograms of their breast density.
Dr. Lehman concluded: “We want women to provide information about their breast density and AI image-based risk score.
“We can do better to inform women about their risk of breast cancer than just looking at a mammogram and saying, ‘It’s dense, it’s not dense.'”
Source link